Osteochondral Debridement/Repair Protocol
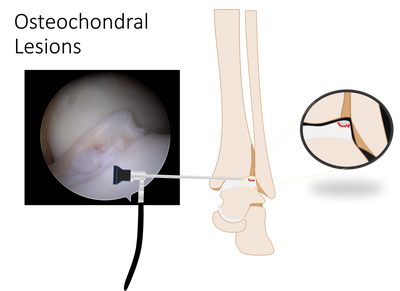
Ankle Arthroscopy with Osteochondral Lesion Debridement and Particulate Articular Allograft
Primary Goals:
- Protect the cartilage repair from shear stress during early healing
- Restore ankle range of motion without axial or torsional loading
- Gradually reintroduce loading and impact in a controlled fashion
Key Restrictions:
- Avoid shear stress across the ankle for the first 6 weeks
- Avoid impact activities for 4–6 months postoperatively
Phase 1: Weeks 0–2
Weight Bearing:
- Non-weight bearing or touch-down weight bearing in a splint or boot (per surgeon preference)
Immobilization:
- Splint or CAM boot at all times except for hygiene and prescribed exercises
Range of Motion:
- Begin ankle range of motion out of the boot
- Active and active-assisted dorsiflexion and plantarflexion only
- Range of motion exercises must be performed non-weight-bearing
Restrictions:
- No inversion or eversion
- No loaded dorsiflexion
- No squatting, lunges, or step-downs
- No pivoting or torsional movements
Other:
- Edema control, elevation, cryotherapy as needed
Phase 2: Weeks 2–6
Weight Bearing:
- Progress to partial weight bearing, advancing to weight bearing as tolerated in boot only
Range of Motion:
- Continue non-weight-bearing dorsiflexion and plantarflexion
- Gentle inversion and eversion may begin at surgeon discretion, performed non-weight-bearing only
Strengthening:
- Isometric exercises in neutral position only
- No resisted ankle strengthening
Restrictions:
- No shear-loading activities
- No closed-chain dorsiflexion
- No strengthening in weight-bearing
- No pivoting, twisting, or uneven surfaces
Phase 3: Weeks 6–10
Weight Bearing:
- Transition out of boot into supportive shoe or brace as tolerated
Range of Motion:
- Full ankle range of motion in all planes
Strengthening:
- Begin closed-chain strengthening
- Progressive loading into dorsiflexion
- Proprioceptive and balance training
Restrictions:
- No running, jumping, or impact activities
Phase 4: Weeks 10–16
Strengthening:
- Advance lower extremity strengthening
- Progress proprioception and neuromuscular control
Conditioning:
- Low-impact cardiovascular conditioning (cycling, elliptical, swimming)
Restrictions:
- No impact loading
- No cutting or pivoting activities
Phase 5: Months 4–6
Impact Progression:
- Gradual return to impact activities as tolerated and cleared by surgeon
- Begin straight-line jogging, progressing to sport-specific drills
Goals:
- Restore strength, endurance, and neuromuscular control
- Prepare for return to full athletic participation
Return to Sport
- Low-impact activities: after 6–8 weeks
- Running and impact activities: no earlier than 4 months postoperatively
- Full return to sport: typically 4–6 months postoperatively, depending on lesion size, location, and clinical progress
This website uses cookies.
We use cookies to analyze website traffic and optimize your website experience. By accepting our use of cookies, your data will be aggregated with all other user data.